Protein disguise could be new target for cancer immunotherapy
Researchers at the Francis Crick Institute have identified a protein
that helps tumours evade the immune system and, in certain types of cancers, is
linked to a poorer chance of survival. The protein could become a target for
future cancer treatments.
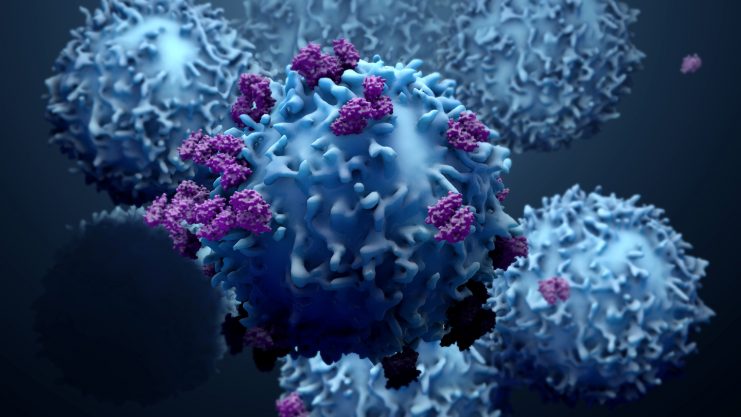
A crucial part of the immune system’s response to cancer is a group of
white blood cells, called CD8+ T-cells, which kill tumour cells. Before they
launch their anti-tumour response, these cells must be told who to attack by
another immune cell, called a dendritic cell.
In their study, published in Cell today (2 June), the
scientists identified a protein that is present in blood plasma and is also
secreted by cancer cells, secreted gelsolin, which interferes with this relay
process by blocking a receptor inside dendritic cells. With no instruction
passed to the T-cells, the tumours avoid their killer response.
The team analysed clinical data and samples from cancer patients with 10
different types of the disease and found that individuals with liver, head and
neck and stomach cancers, who have lower levels of this protein in their
tumours had higher chances of survival.*
They also found that blocking the action of this protein in mice with
cancer increased their response to treatments including checkpoint inhibitors,
a major immunotherapy.
Caetano Reis e Sousa, author and group leader of the Immunobiology
Laboratory at the Crick, says: “The interaction between tumour cells, the
surrounding environment and the immune system is a complex picture. And
although immunotherapies have revolutionised the way certain cancers are
treated, there’s still a lot to understand about who is most likely to benefit.
“It’s exciting to find a previously unknown mechanism for how our
body recognises and tackles tumours. This opens new avenues for developing
drugs that increase the number of patients with different types of cancer who
might benefit from innovative immunotherapies.”
This work builds on the team’s research into dendritic cell biology.
These cells absorb debris from dead cancer cells and hold them internally in
pockets called phagosomes. Binding to a protein on the debris, F-actin,
triggers these pockets to burst, releasing the debris into the cell where they
can be processed and moved to the surface to signal the presence of a tumour to
nearby T-cells.
When the researchers examined the activity of secreted gelsolin, they
found the protein outcompetes a key dendritic cell receptor, blocking its
ability to bind to F-actin and therefore the ability of the dendritic cells to
initiate a T-cell response.
“Dendritic cells play a vital role in the immune system and our
body’s response to cancer,” says Evangelos Giampazolias, author and
postdoc in the Immunobiology Laboratory at the Crick. “Understanding this
process in more detail will enable us to identify how cancers are able to hide
and how we might remove their disguise.”
Oliver Schulz, author and research scientist in the of the Immunobiology
Laboratory at the Crick says, “While secreted gelsolin circulates in
healthy blood plasma, some cancer cells secrete really high levels of it — so
these tumours are launching an anti-immune defence which helps them avoid
killer T-cells.
“Reducing levels of this protein will help alleviate the
competition for binding to F-actin and allow dendritic cells to communicate
their vital message.”
The researchers will continue this work, trying to develop a potential
therapy that targets the secreted gelsolin in the tumour without affecting the activity
of this protein in other parts of the body.
Journal Reference:
- Evangelos
Giampazolias, Oliver Schulz, Kok Haw Jonathan Lim, Neil C. Rogers, Probir
Chakravarty, Naren Srinivasan, Oliver Gordon, Ana Cardoso, Michael D. Buck,
Enzo Z. Poirier, Johnathan Canton, Santiago Zelenay, Stefano Sammicheli,
Natalia Moncaut, Sunita Varsani-Brown, Ian Rosewell, Caetano Reis e
Sousa. Secreted gelsolin inhibits DNGR-1-dependent cross-presentation
and cancer immunity. Cell, 2021; DOI: 10.1016/j.cell.2021.05.021